One of the greatest challenges we face during the Covid-19 pandemic is dealing with the abnormality of not being able to safely share indoor spaces with people who may, or may not, be infected. Indoor environments carry a particular risk if the SARS-CoV-2 virus that is responsible for Covid-19 is transmitted as aerosols through air which is trapped for a relatively long time in enclosed spaces.
Covid-19’s Aerosol Threat
On September 10, 2020 Dr. Anthony Fauci, director of the NIH National Institute of Allergy and Infectious Diseases, reported in a Harvard Medical School Grand Rounds webcast on the status of Covid-19 transmission that “The aerosol and particle physicists that have approached us now have told us that we really have gotten it wrong over many, many years. Bottom line is, this is much more aerosol than we thought.” He went on to explain that the medical community had been defining the maximum size of an aerosol – a particle small enough to float around in the air for a long time – to be about half that of actual aerosols, including those emitted by a person when they are talking (or just breathing).
For me, this revelation of aerosol classification was not news. What I did find surprising was that medical researchers had been misidentifying the size of aerosols when the physics and methodology for determining the size of aerosol particles and droplets has been in textbooks for decades. In fact, the scientist who essentially defined an aerosol, J.J. Stokes, published his work on the subject in 1851. Physicists are not the only ones who have known this. As a graduate student in mechanical engineering in 1997, I was studying droplet sprays similar to what comes from a cough and spent many hours characterizing how the different sized droplets moved around in a turbulent air stream as they evaporated. Many of the papers I have read on cough sprays were done through university engineering departments, such as this one showing mask effectiveness which was published in June 2020 in the journal Physics of Fluids.
A Multidisciplinary Approach
The effort to figure out how to keep people safe from the Covid-19 virus in public is daunting and multidisciplinary. It requires action from a wide range of top experts in virology, epidemiology, chemistry, fluid mechanics, and other specialized areas. Programs within, or sponsored by, the CDC and NIH are supposed to bring together these knowledge sources to determine all the different mechanisms for transmitting a virus from one person to another through the air, contaminated surfaces, personal contact, or some other means.
Success in the war on Covid-19 is also dependent on the organizational directors, like Dr. Fauci, who oversee these concerted battles, as well as the journalists, politicians, and public safety authorities who provide critical information links between what the experts know and how that knowledge is used to protect the public. If too many of them make uneducated decisions or pass along misinformation resulting from bad assumptions or misinterpretation of research, the value of the work of the experts is greatly diminished. And if those in the most influential roles of government promote disinformation instead of responsibly guiding everyone through the uncertainties of the pandemic, expert analysis and advice has to compete with dangerously absurd speculation.
This is why it is crucial that the experts have a realistic grasp of the limitations of their own research and knowledge when responding to questions. There should be no expectation that any given doctor is also an epidemiologist with insights into how the price of chicken in Thailand may be an indicator of a virus outbreak in Southeast Asia. Likewise, asking an epidemiologist with no clinical experience to diagnose your sinus headache doesn’t make sense. I’m not sure if it is even possible for a single person to have true expertise in every discipline involved in fighting a pandemic, so it is imperative that journalists, government officials, and the public not expect Dr. Fauci or any other advisor to necessarily have all the specific answers at hand. Such spokespersons have a responsibility to refer specific questions to individual experts, including engineers and physicists who have been studying the fluid dynamics of sprays for many years. We often want one person that we trust to have all the answers, but that is an unrealistic expectation.
I want to emphasize these points about expertise before diving into a discussion of airborne SARS-CoV-2 transmission that falls into my own knowledge area. Since I have no formal medical training, my explanations of how virus particles travel through air and some potential remedies must be limited to my education and professional experience in spray behavior and fluid dynamics. This examination begins at the point when droplets exit someone’s mouth and stops where they land on a surface, get caught in a filter, or are exhausted to the outdoors. It is just one part of the puzzle, but a critical one as Dr. Fauci emphasized, that will allow us to figure out the safest way to get people back into public buildings.
Airborne Virus Transmission
You have questions.
The trillion-dollar question of 2020 is how exactly does the SARS-CoV-2 virus jump from one person to another and what is the best way to stop that from happening? Right now, stopping the airborne virus literally means putting up physical barriers, including space, fabric and other sundry filters, plastic sheets, and walls. But with a better understanding of how the virus is transmitted, can we apply a dose of innovation and improve that list of barriers?
What is needed to make classrooms, offices, restaurants, and auditoriums safe for occupancy? For public buildings, guidance usually comes from the American Society of Heating, Refrigeration, and Air-Conditioning Engineers (ASHRAE) and local building and health codes. But are those standards and rules good enough?
Then there are the challenges of actually getting to another building from your home without being exposed to the virus. The number of people who rely on public transportation for at least some portion of their commute is not insignificant and should be taken seriously, especially when it comes to children depending on virus-free busses to get to school. Even if a bus is 100% decontaminated before everyone gets on, will the virus particles from an infected rider get vented out before floating past or landing near other passengers?
We should start looking for answers by first asking one more question: what do we already know about virus transmission through the air and how do we know it?
Fortunately, we have the technical ability to look directly at the physical details of an infectious SARS-CoV-2 particle which is a fairly spherical assembly comprised of the virus RNA strands surrounded by a fatty lipid envelope that also incorporates a few different specialized proteins that help with the infection process. When the entire package is intact, it is infectious and called a “virion”. When hunting down virus particles, researchers will mostly come across separated virus RNA or broken envelope proteins, but it is the intact virions that we are concerned about. This species of coronavirus is new and unique, but it is not entirely different from many other viruses, so we can lean on 90 years of virology and fluid mechanics research to get a pretty good picture of how an airborne virion moves from one person to another.
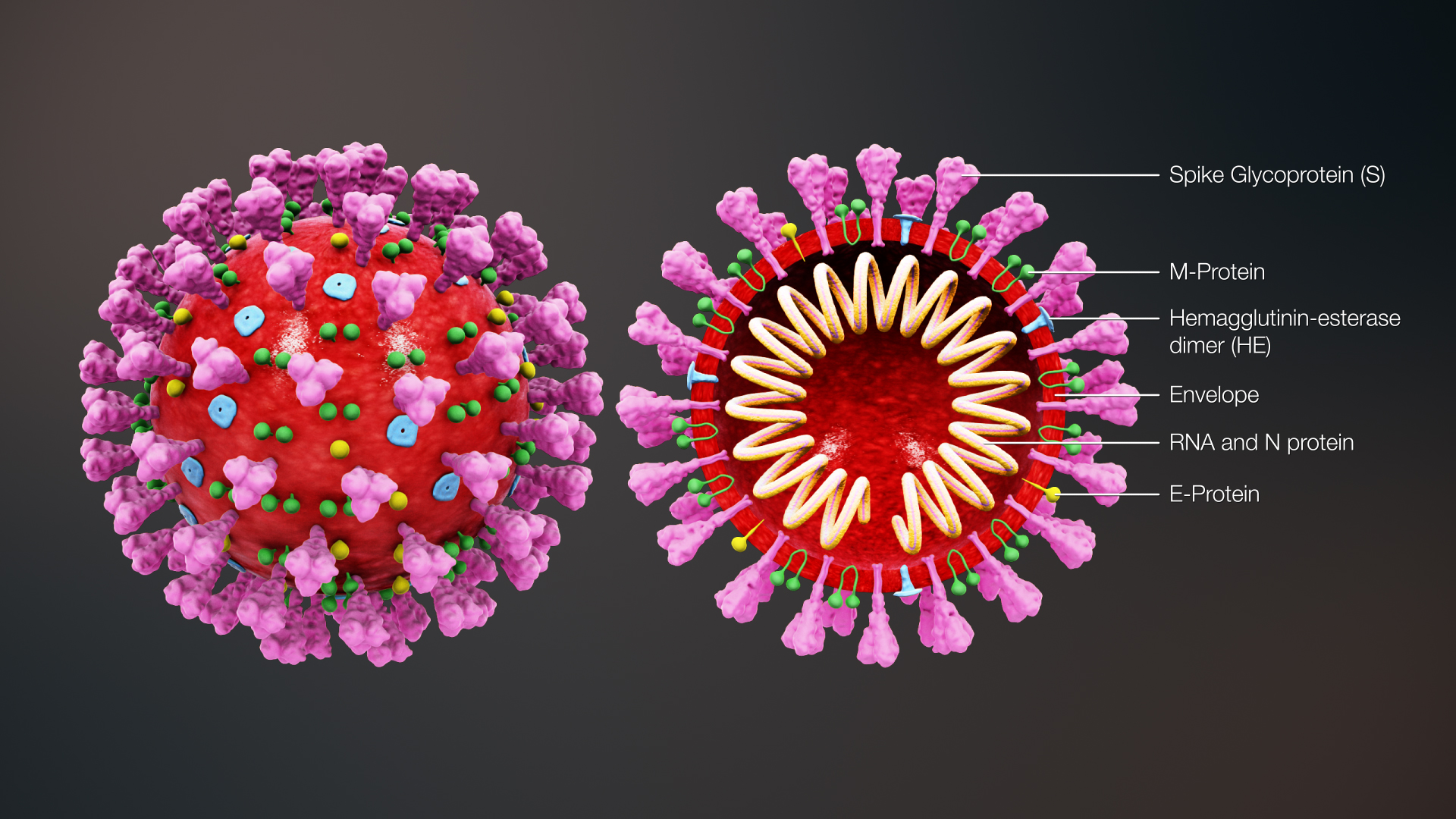
Image: Scientificanimations.com via Wikimedia / CC BY-SA 4.0. Rendering of a SARS-CoV-2 virus virion. It is approximately 0.1 micrometers in diameter. The spikey proteins are what attaches to a cell in order to infect it. Note: The Envelope (shown in red) supports the spherical shape of the shell and is made of a fatty lipid structure that attaches to soap or detergent. Wash your hands!
SARS-CoV-2 Basics
Let’s take a look at the basics. There are several things that we know for sure:
- SARS-CoV-2 virions travel in droplets expelled through exhalation and sneezing (as well as other bodily fluids that tend not to get projected into the air).
- A SARS-CoV-2 virion is submicroscopic (about 500 times smaller than the width of a human hair) such that it has almost no influence on even the smallest droplet that is transporting it. This means we can focus on tracking the droplets as if they did not contain virions.
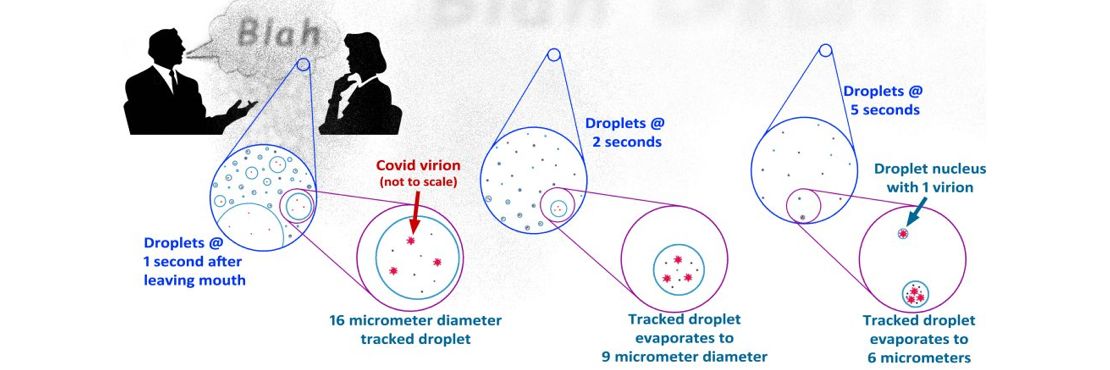
- Droplets that get launched from your mouth when you talk contain more than water. About 1% of a typical size droplet contains proteins, mucus, epithelial cells, white cells, electrolytes, random small molecules, and possibly an infectious virion or two. Estimating a realistic number of virions per droplet, or how many are needed to cause infection, is an area of ongoing research and a really great question for a virologist. For purposes of this discussion, I am using the conservative assumption that most droplets that are at least 2 micrometers in diameter (droplets smaller than about 10 micrometers are aerosols) have at least one virion.
- Droplets evaporate at a predictable rate, depending on their initial size, velocity, and surrounding temperature and relative humidity. Saliva droplets only evaporate until they reduce to a tiny clump called a “droplet nucleus” that contains the proteins, mucus, epithelial cells, white cells, electrolytes, random small molecules, and an approximately equal amount of water molecules that remain attached, according to a study conducted in Germany earlier this year.
- Big droplets drop; little droplets don’t drop but instead go with the air flow as aerosols. Big droplets are the ones that typically fall to a surface somewhere between 2 and 6 feet (or more for big sneezes) of a person’s mouth if they are not wearing a mask – these droplets never make it past a tight-fitting mask. Tracking the droplets is a 2-step process of following the initial emanation of talking/yelling/laughing/coughing/sneezing, which has enormous variability, and estimating the subsequent long-range or “far-field” travels of the nucleus aerosols.
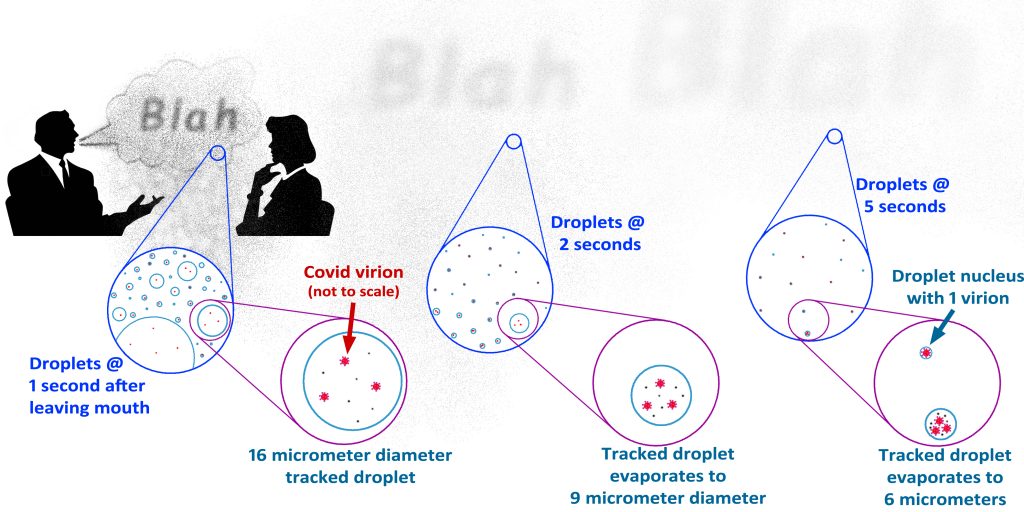
Image: Chris Wark. This illustration shows how exhaled droplets with SARS-CoV-2 virions evaporate as they travel. The largest droplets fall away within a second or two, but smaller droplets stay in the air longer. The droplet shown as being “tracked” starts out large enough to not be considered an aerosol, but it quickly evaporates to a size that is an aerosol and can stay in the air for a long time as it continues to evaporate down to a “nucleus”. These smaller aerosol droplets disperse and go with the air flow until hitting a surface like an air conditioning filter.
I should note that the debate over whether Covid-19 is spread through the air or by contact with surfaces has a lot to do with the size of droplets that the SARS-CoV-2 virions are typically found in. If we had reason to believe that infectious virions were almost exclusively in large droplets, then yes, it would make sense that transmission through surface contamination would be of singular concern. But the research so far seems to confirm that nearly all the virions exit in droplets of all sizes larger than 5 micrometers.
- Masks work – even the simplest thin cloth masks. If nothing else, masks dramatically slow the velocity of air being exhaled or coughed from your mouth so that the small droplets that do make it through the mask do not get projected into someone’s face but are immediately aerosolized and washed away if there is adequate ventilation, such as being outdoors. How well a mask captures droplets depends on a number of factors that are still being researched. Some of these studies can seem a little misleading if they ignore how exhaled air flows between face and mask (your breath doesn’t just go straight through the mask), ignore how breath moisture improves the filtering characteristics of a mask, count droplets smaller than 1 micrometer, oversimplify the description of the fabric in virtual studies, or do not take into account how well the mask seals around the face. It doesn’t mean they are wrong, just that simplifications need to be recognized and disclosed, especially when translating a study’s conclusions for the general public.
- Even aerosols containing a virion can collide with a surface, making that surface infectious. Regardless of measures taken to block, capture, or vent virions, surfaces in public or critical areas should still be cleaned regularly as if they were contaminated. As we will see, the trick is to “flush” the virion-laden air away in the shortest distance possible before they can interact with another person or surfaces that nearby people are touching.
- Outdoors, the effective ventilation of the space in and around a group of people is many times better than typical indoor spaces.
There are also a few things that have been studied extensively but are difficult to characterize:
- What is the absolute minimum “safe” distance from someone not wearing a mask? Is it 3 feet, as the WHO (World Health Organization) was recommending at one point, 6 feet, as is commonly required, or 24 feet as some scientists are now warning? The basis for each of these distances is fairly well grounded in numerous studies that have been conducted for nearly 90 years. In rather crude terms, these three distances represent how far a clump of air and large droplets travel when talking, coughing, or sneezing, respectively. But even those divisions are too simplistic. A person with a strong voice talking very loudly will project droplets up to 6 feet while someone with weak lungs may only project a cough a couple of feet. Some of the studies that try to correlate projection lengths with categories of types of people are fascinating but produce questionable results. Sneezing data is all over the place – from 6 feet out to 24 feet. However, sneezing directly at people has never been tolerated, so the long distance a big sneeze might cover really should not be included in the same context as reasonably safe distances for people to talk to each other. More important is that all these safe-distance recommendations assume no ambient air flowing around the people, which can increase or decrease these “safe distances” quite a bit.
- Except in highly controlled environments, it is usually difficult to predict how thoroughly and quickly the air around a person who is indoors is actually getting replaced. At least when outdoors, the quantity of air moving around is so huge that an effective amount of flushing of droplet-laden air can be assumed when people are staying several feet away from each other (further if they are yelling or beer is involved). Indoors, the amount of air that can be assumed to flow past people depends on a wide range of factors, most of which are rarely known without some advanced analysis. It should also be noted here that circulating air is not the same as ventilating it. If a stand-alone or desk fan is blowing in a room, it doesn’t make aerosols leave the room, it just makes them swirl around in it until they land on a surface or eventually go out through a vent or window.
- Estimating how many active coronavirus virions are in the air of a given space has been almost impossible in the past, though very recent breakthroughs in virus collection technology are making it much easier. The two primary challenges in counting virions are that 1) they are extremely small and 2) they are fragile and usually get damaged during collection, making it difficult to estimate how many were fully intact before collection, thus infectious, and how many were already broken up within the droplet. In the past, recommendations for dealing with virus outbreaks had to be based on assumptions derived from samples of damaged virions. Improving methods of quantifying virions will be particularly important for distinguishing the threat of surface contact transmission from that of airborne transmission. Again, an expert understanding of the collection of virions and its current state of development is found in the realm of virology. I only mention this because I believe it is important to note how accurate the accounting of virions in aerosol droplets is when trying to determine the type of airborne threat they pose and what the most effective barrier and ventilation solutions will be.
Exhaled Breath Outdoors
Before getting into the current state of indoor air ventilation, let’s look at what happens to your exhaled breath outdoors. First, it is helpful to get a feel for a couple of technical measures, such as wind speed, and the time it takes to wash virions away before reaching another person. Did you feel that breeze? Not quite or just barely? Then, according to the Beaufort Wind Scale that is used for weather events, that very light breeze is air moving at approximately 5 mph. At that speed, a clump of air moves past your face in less than half of a second.
When you are talking normally to someone who is 6 feet away, the sound waves reach them almost immediately, but the puff of air from you loudly pronouncing the letter “p” takes a little less than 2 seconds to go that far. But wait, if the breeze flows across your face in 0.4 seconds, how does that puff of air ever reach the other person? It doesn’t! In fact, even if the breeze is so slight that you cannot feel it, say 2 mph, the air is still moving fast enough to flush the virions away.

Image: Chris Wark
Two mph is another good reference point as that is approximately how fast air needs to move to make a candle flame flicker. Here is a fun experiment that you can do to get a good feel for how far your breath travels when you talk, yell, or cough:
In a very still room, light a candle – preferably a taper on a skinny candlestick – and position it on a table about 1 foot from your face. Start talking in a normal voice and you will see the flame jump a lot. Now move it 2 feet away and see if the flame shudders when you talk normally or yell. Then 3 feet away and see what happens when you yell or cough. Now move the candle 6 feet away and see if the flame flickers when you cough (note the delay from the time you cough to when you see the flame react). Have someone else do the experiment and see if the results are the same. When the candle flame just barely flickers, the aerosols (mainly droplet nuclei at that point) in your breath keep traveling a few inches farther than the candle before wandering off in other directions.

Image: Wendy Wark. Please ensure that you have proper supervision whenever conducting an experiment where fire is involved – safety first!
Ah, but what if the outdoor breeze is blowing into or away from my face or into someone downwind? Good point. This is the one aspect of being outdoors that poses a risk. Fortunately, wind rarely flows so directly and actually swirls and mixes a lot more than we are aware of. This disperses aerosols, making them less likely to reach another person; but it also means that it’s not a bad idea to wear a mask outside if you are going to be within just a few feet of other people in any direction.
Indoor Air Ventilation
Now let us compare being outdoors to what is experienced indoors. The most important thing to understand is that standard HVAC (heating, ventilation & air conditioning) systems for schools, offices, restaurants, stores, gyms, and auditoriums are not necessarily designed for removing virus-sized particles from the air. Building codes require commercial HVAC to bring inside a certain amount of outdoor air (ventilation), but those rules are only meant to keep CO2 concentrations below a prescribed level. For most HVAC systems, while conditioning a space with cold or warm air, the air blowing through the room is mostly re-circulated and the required outdoor air is mixed in such that it may make up only a small portion of the total HVAC air flow.
However, the air circulating through a building’s HVAC system is supposed to be filtered. In fact, the air filtering requirements in most locations in the U.S. are effective enough to remove a little less than half of particles the size of a typical saliva droplet nucleus. Many locations now require or provide incentives to use filters that can trap about 75% of the nuclei when properly maintained. Filters that catch nearly all nuclei flowing through the system are commercially available, though rarely installed because of the higher maintenance and greater power consumption of the circulation fans.
The total filtered and conditioned circulating air flow through a building will vary depending on the local climate, how a given space is being used, and how the HVAC fans are controlled. Within a reasonable range, we can at least get an idea of how indoor circulation compares to being outdoors through the use of ASHRAE guidelines for HVAC design.
The minimum volumetric flow rate of outdoor air, or ventilation rate, required for office spaces by ASHRAE (the standard for nearly all building codes in the U.S.) is equal to about 80 times the breathing rate of an average adult sitting at their desk. So, CO2 levels are well regulated. But when it comes to meeting our challenge of removing SARS-CoV-2 aerosols from the air around each occupant, we have a problem: this required ventilation flow rate is only 0.2% of what is needed to completely flush the air between two people sitting 6 feet from each other before their virions can reach each other. In reality, the HVAC engineering best practice is to set minimum air circulation at 3 to 6 times the required ventilation rate, but that still only gets us to 0.6% to 1.2% of the flow rate needed to flush SARS-CoV-2 from between 2 occupants.
Why not just increase the building air flow? Moving more air means increasing the size or number of the fans and fans use energy. More or bigger fans and the additional electricity to run them can be expensive, so flow rates are generally kept as low as possible.
In a classroom, higher ventilation rates are required, typically resulting in flow rates about 5 times higher than for an office space, but still only around 5% of what we need flowing past each student, assuming they are all 6 feet away from each other. And then after the air flows past one student, what keeps it from continuing on past another student and another and then the teacher on its way to the exhaust vent?
The issue is that these engineering standards are for an entire room and largely ignore what happens at each spot where someone is sitting. Even if the room was designed with an average flow rate of our outdoor example, the local flow rate might not be nearly good enough. Depending on the shape of the room and where you put furniture, equipment, desks, people, etc., that “fresh” air might head for the exhaust vent along one wall while leaving stagnant pockets in an opposite corner. For the person sitting in that stagnant pocket all day, it could be a serious health issue.
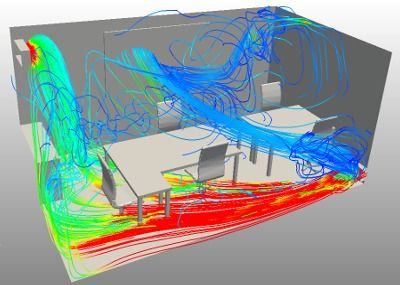
Image: SimScale. Computer modeling of air flow is known as Computational Fluid Dynamics (CFD). This CFD model shows how uneven air flow can be in a typically air conditioned small enclosed office.
Besides walls and furniture, there are also thermal effects that can strongly steer air flow because warm air rises and cold air drops. In fact, one of the most common drivers of air moving around a single person sitting still is that person’s body heat causing the air next to their skin to rise and pull lower air up with it. In fact, one well-known ventilation strategy called “displacement ventilation” specifically takes advantage of the heat rising from people and computers to create a vertical flow throughout most of the space.
Windows for Ventilation?
So, the best thing is to open some windows, right? Most residential building codes in the U.S. assume that all ventilation for a home will be achieved by opening a window, although some recent code revisions, such as in NYC, are finally requiring supplemental ventilation under certain conditions. Those same codes will require exhaust fans for bathrooms and possibly kitchens, but the air that goes up into an exhaust fan must come from somewhere and that somewhere is through open windows. The problem is that the outdoors right outside your home is too often too cold, too noisy, too dusty, too hot, too smelly, too stormy, too….something, to leave open. Counting on people to open windows to maintain a healthy environment in their home, office, or classroom is short-sighted at best and dismissive at worst.
Another problem with depending on windows for ventilation is that it assumes the wind will always blow and that a breeze will make its way to the other side of the room. I have done numerous studies of strategies for architects to effectively use open windows for ventilation and it only works when the building is specifically designed to take advantage of natural ventilation. Some great examples of how this has been done are buildings in warm to moderate climates designed and built before the advent of air conditioning. They typically provided a way for the wind to blow all the way through the wing of a building by way of transoms above the doors.
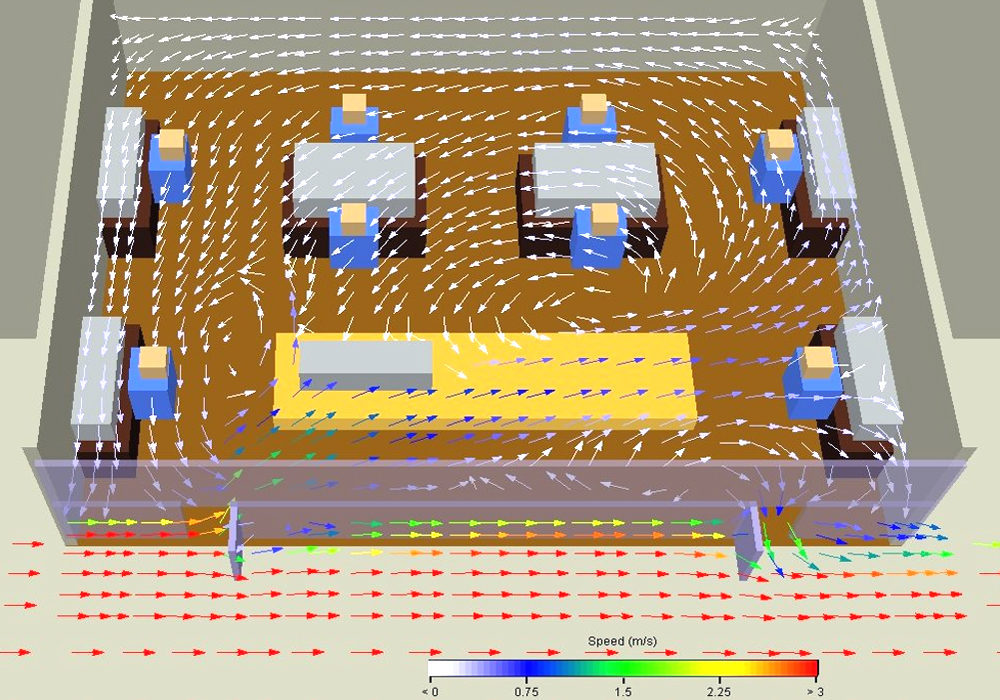
Image: Chris Wark. This CFD model demonstrates the effectiveness of “blind” natural ventilation where windows on the same side of a building open outward to catch the wind. Note how the wind flows fairly well near the exterior wall, but poorly toward the interior wall.
Speaking of bathroom vents, the New York City Department of Education recently conducted a room level inspection of every public school building in NYC and found that less than half had usable restrooms. I think the problem is worse as my experience has been that nearly all restroom exhaust fans are impressively undersized in commercial and public buildings. But they almost always meet code so everything should be fine with the air quality in public restrooms, right? Wrong. Public restrooms stink. And if they don’t smell like…you know…then they just smell weird and that is bad because it means it is an unhealthy environment.
The amount of exhaust most building codes require for restrooms replaces the air every 7 to 8 minutes. Or to frame this in the description of how thoroughly air flows past a person outdoors, it is very similar to being in a 0.02 mph “breeze”. Not only is it exceedingly unpleasant, it means any SARS-CoV-2 aerosols that get released in a restroom are hanging around for several minutes – plenty of time to infect the next victim. Restrooms are small spaces and there is little reason to compromise on upgrading the ventilation of them, especially when you consider that the cost of a commercial exhaust fan with 10 times the flow rate of a $200 code-compliant fan is about $300.
Better Indoor Environments
We know that indoor environments need to be controlled better if we are going to ensure that students and teachers are safe from Covid-19 in classrooms, workers are safe in office spaces, elderly people are safe in nursing homes, people are safe in restaurants and auditoriums, and that people who live in high-density housing have healthy air in their own homes. Fortunately, we have quite a few specialized HVAC applications to look at for some creative solutions, some of which were developed specifically to deal with situations not unlike the Covid-19 pandemic.
Probably the most critical type of ventilation application that I have been involved with was the CFD computer modeling of air flow through airports, embassies and other government buildings in response to the “weaponized” anthrax attacks that occurred following the 9/11 attacks. The concern was that aerosolized anthrax could be released from a package or bag dropped in the lobby of one of these buildings. The job was to figure out how to keep the anthrax aerosols isolated and vented away as quickly as possible before seriously infecting anyone. The solution in this case usually involved controlling differences in air pressure between adjacent rooms and providing separate, high-flow ventilation systems for each room, but became more complicated in large spaces such as airports.
A similar application is the ventilation of smoke from a fire. Many buildings, particularly high-rise buildings have a separate set of high-flow exhaust fans and control strategies specifically in case of a fire, although these fans would also be used if there was a sudden extreme exposure to other noxious fumes that might come from, say, a chemical spill in the building. Flushing smoke out of a building is certainly a different situation than keeping a space Covid-free, but there is a lot to learn from studying the physics of where smoke aerosols go (or don’t go) during and after a fire.
A few other examples of special, or even critical, air flow requirements that I believe are useful for finding SARS-CoV-2 venting solutions include big computer rooms, grocery stores, and laboratory clean rooms:
Computer rooms, data centers – Air circulates from tiles throughout the floor up past the computer racks to the ceiling. This is for cooling rather than particulate filtering, but the concept that needs to be stressed here is that it flows from the floor to the ceiling to remove heat quickly without the hot air flowing into another computer rack, just as we want to keep nuclei containing SARS-CoV-2 virions from flowing from one person to another. It takes advantage of the concept of displacement ventilation that I mentioned earlier – use the buoyancy of warm air to help carry away the virus vertically instead of past other people. Putting in the type of raised floor found in computer rooms is expensive and difficult, but there are other cheaper ways to introduce air along the floor that are nearly as effective.
Grocery stores – I include grocery stores because they all contain a familiar example of another strategy that can be extremely effective for isolating spaces. Modern open refrigerated cases use what is called an air curtain to isolate the cold products from the warm room by blowing cool air from a long skinny diffuser at the top front edge of the case down toward another long skinny return grid at the bottom edge of the case opening. The warmer air from the rest of the store simply gets pulled down along with the air curtain air back into the return grid. I have done measurements and computer modeling of them and these air curtains are really very effective when the return grids are not blocked. Again, even though this example for thermal purposes, it also works equally well where the idea is to isolate the clean air in one space from SARS-CoV-2 contaminated air in another space. Air curtains are also used at entrances to buildings and corridors where environmental isolation without doors is desired.
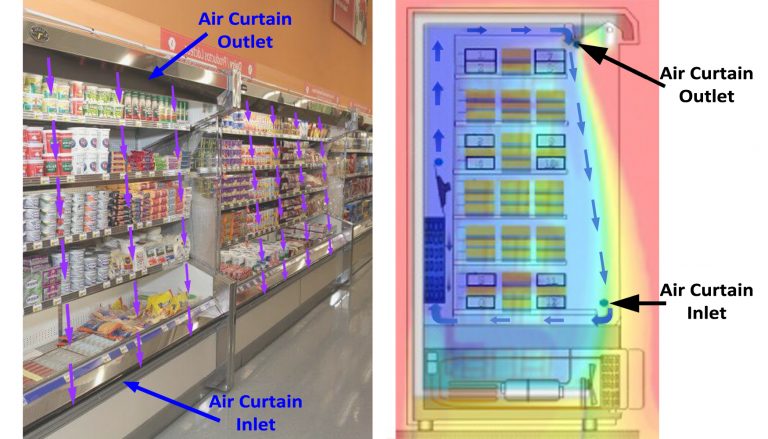
Images: Uncredited and modified by Chris Wark. Modern open refrigerated cases use air curtains to isolate the cold products from the warm ambient store air. The constant sheet of flowing air will block aerosols as well as warmer air. The same strategy can be used to create room barriers to SARS-CoV-2 contaminated air.
Clean rooms – This is a broad category that includes a variety of laboratories, semiconductor manufacturing, pharmaceutical processing, etc. In this case, the entire purpose of the facility is to minimize, if not eliminate, all particulates of every size from the room air. Where simply increasing HVAC circulation rates through special air filters is not enough, considerable attention is given to where the air flows throughout the room so that no particulates can get stuck in stagnant work areas. Strategies for achieving this include both vertical air circulation (floor-to-ceiling or ceiling-to-floor) and air curtains to isolate doors or non-essential perimeter areas. The techniques used in clean rooms could translate to less demanding spaces such as classrooms by relocating air grills and installing an air curtain between the teacher and students instead of using a clear plastic barrier which blocks sound and can be scary for younger children.
These are just three of the many high-performance HVAC applications that come to mind and no stone should remain unturned when looking for affordable, creative, ways to protect building occupants from Covid as well as any other pathogen with the potential for causing local epidemics. Unfortunately, the two primary reasons buildings, especially schools, are not already designed or retrofitted with these measures are cost and professional risk which can limit creativity. The building industry is driven by codes, standards, and incentives provided by government entities and utilities, but exceptional design conditions or occupancy requirements are needed for a building owner to exceed those requirements and guidelines.
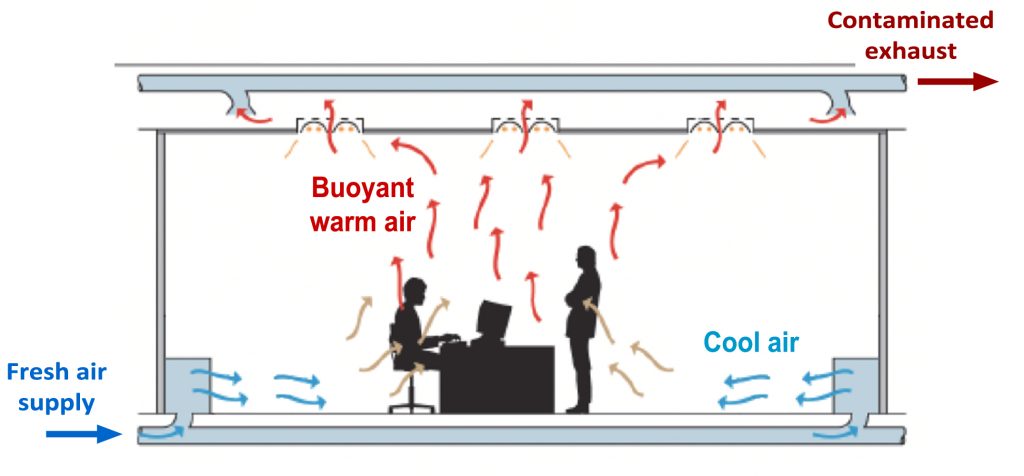
Image: Modified diagram from TheGreenAge. This illustration of “displacement ventilation” shows how exhalation-contaminated air can be flushed away above peoples’ heads before flowing past other occupants.
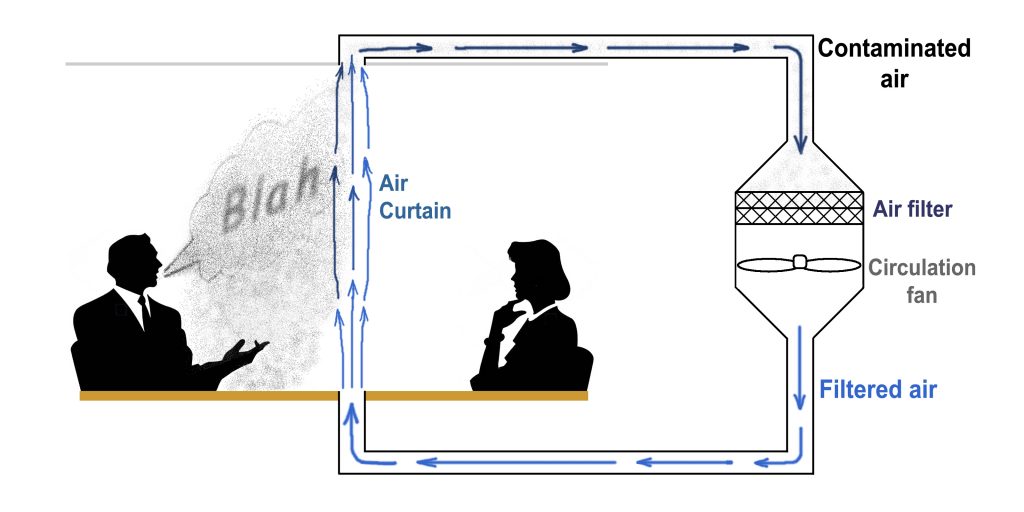
Image: Chris Wark. One possible solution for isolating and removing SARS-CoV-2 virions in meeting rooms is the installation of an air curtain directly into conference table or between desks.
In many cases, the extra cost of, say, an underfloor room air supply like the ones often found in computer rooms, may very well be justified if not already designed into the building. But immediately dismissing the overall strategy of an improved displacement-style ventilation with higher flow rates and air curtains because the cost is assumed to be prohibitive is irresponsible. When engineers with expertise in room air flow are brought in, a wide range of options become available for efficiently introducing fresh air at strategic locations and exhausting it in a way that maximizes indoor environmental quality. I have done exactly this for many clients looking to deal with specific environmental challenges in buildings ranging from new museums to old landmark office buildings.
Safer Air in Buildings and Public Transportation Needed
So far, I have only talked about buildings and have not mentioned ventilation in planes, trains, or automobiles. From an engineering and physics standpoint, they are basically just tiny buildings that move. The same fundamental strategies apply, just on a smaller scale. Modern airplane cabin ventilation is not bad because it has to accommodate so many people packed into such a small space and the risk of health and safety mishaps must be minimized while in the air. Airplane filtration is very good, but the flow rates are low and could be directed more effectively. It is a similar situation for most modern rail where the windows cannot be opened. Older trains need help. Cars are more like a home in that ventilation is pretty much left up to the occupants. School busses are a problem and need to be improved. They need to be retrofitted with vertical flow ventilation for each row so that virions from potential yelling and coughing in one row is vented directly away without infecting children in the next row. Such solutions would also minimize the spread of other pathogens beyond coronaviruses.
We are now in an era where the cost benefit analysis of building upgrades takes on a whole new set of factors, where the bar for minimum air quality standards has just been raised considerably. What is the cost of installing the necessary additional vents, ductwork, and upgraded fans/filters compared to the cost of leaving an office space empty indefinitely? What is the cost to a city for increasing the effectiveness of its HVAC system, ensuring the health and safety of students and teachers, compared to the cost of compromising education and increasing the burden on parents?
Communities need to commune for many reasons and the cost of prolonged isolation and social-distancing has yet to be fully realized. If we want to limit that cost, government and business leaders must have the courage to invest in innovative solutions for making the air in buildings and public transportation as safe as possible.
~ Christopher G. Wark
See my article originally posted on September 27, 2020 at Wark Energy Consulting.
Publisher’s Note:
Read Greenroofs.com collaborator Chris Wark’s 7-part Green Roof Energy Series which originally ran from April 5, 2010 through April 28, 2011. His “Cooler than Cool Roofs: How Heat Doesn’t Move Through a Green Roof” explains the key aspects of green roof heat transfer issues and the best ways to take advantage of a green roof’s energy benefits.

Christopher Wark is Principal of Wark Energy Consulting and the founder of Ponix MicroAg LLC, a development-stage company that is creating a line of compact plant enclosures for the CEA market. Chris has over 30 years of multidisciplinary engineering experience providing mechanical, analytical, and electronics support and services to manufacturers, universities and national labs. He holds Bachelor and Master of Science degrees in Mechanical Engineering (with a minor in Materials Science) from Washington State University where his graduate work focused on thermodynamics, fluid dynamics, and combustion.
For the past 19 years, Chris has focused his efforts on the development and promotion of technical solutions in architecture and construction. He has provided energy and environmental quality analysis, CFD modeling, and LEED consulting services for several engineering and building consulting firms in New York and California. In 2002, Chris established SHADE Consulting/Green Roof Innovations (GRI) with his wife Wendy.
With GRI, Chris developed several innovative modular eco-roof systems and in 2010, Chris designed a modular planting system in partnership with Guiyang Chuangjia High-Tech Accelerator Co. LTD in Guiyang, China. In Guiyang, he saw how most of the apartment balconies and rooftops were filled with vegetable gardens. The idea of providing an improved environment for food production in built environments, along with key GRI design concepts, inspired the development of the patented pPod™ miniature greenhouse developed by Ponix MicroAg.
Contact Christopher Wark at: cwark@pponix.com, 917-565-6919.
 Greenroofs.comConnecting the Planet + Living Architecture
Greenroofs.comConnecting the Planet + Living Architecture






Safer Space in the Age of Covid-19 – Greenroofs.com – New Zealand Online News
[…] Click here to view the original article. […]
Safer Space in the Age of Covid-19 – Greenroofs.com – Latest CoronaVirus Information
[…] Safer Space in the Age of Covid-19 Greenroofs.com ” “covid-19″ when:1h” – Google News […]
Safer Space in the Age of Covid-19 – Greenroofs.com – SupremaA.com
[…] One of the greatest challenges we face during the Covid-19 pandemic is dealing with the abnormality of not being able to safely share indoor spaces with people who may, or may not, be infected. Indoor environments carry a particular risk if the SARS-CoV-2 virus that is responsible for Covid-19 is transmitted as aerosols through air which is trapped for a relatively long time in enclosed spaces. Covid-19’s Aerosol Threat On September 10, 2020 Dr. Anthony Fauci, director of… Safer Space in the Age of Covid-19 – Greenroofs.com […]